An antibiotic used to treat severe infections shows promise against a very resistant and deadly form of tuberculosis. XDR-TB is resistant to at least four of the drugs used most often against the disease.
Extensively drug resistant tuberculosis – or XDR-TB – is still considered rare, although cases have been reported in nearly 80 countries. Health officials believe the number of XDR-TB cases is underreported because there’s no specific test for it.
It can be cured, but the odds against that happening are often quite high. It can kill quickly, especially if a person is co-infected with HIV, the virus that causes AIDS.
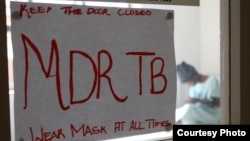
Dr. Ray Chen, a staff clinician at the National Institute of Allergy and Infectious Diseases, says XDR-TB is the next step after MDR-TB, or multi-drug resistant tuberculosis, which is a lot more common.
“That’s been a known problem for many years, primarily as a result of people who don’t take their drugs well. And then the tuberculosis bug slowly develops resistance to the drugs that are used,” he said.
MDR-TB is resistant to two of the top line drugs used for standard tuberculosis therapy. When the disease becomes resistant to two additional first-line drugs, it’s upgraded to XDR-TB.
“It came to world attention in 2006 in a study in South Africa where a number of patients were found to have this extensive resistance to tuberculosis drugs, and they had a very high mortality rate. And so it became recognized as a major problem for tuberculosis,” he said.
In fact, the mortality rate was as high at 90 percent in patients also infected with HIV.
Standard TB treatment can take up to six months. MDR-TB treatment can last between 18 and 24 months.
So researchers knew that more drugs were needed to tackle the various forms of TB. They had heard of some informal studies using the drug linezolid on TB patients with some success. But there was no formal study.
Linezolid is a drug that’s already on the market and it’s approved for the use of resistant bacteria, which we call gram-positive bacteria that don’t respond to typical antibiotics.
To find out, researchers tested linezolid on 41 patients with XDR-TB. The patients already had been treated for six months with the best TB drugs available, but failed to respond. Chen said linezolid was added to their regimen.
“We found that adding the linezolid had a significant effect and that most of the patients converted their sputum from showing tuberculosis to not having tuberculosis in the sputum by six months. About 87 percent of the patients became negative for tuberculosis within six months. So it showed a very good response,” he said.
That’s the good news. The bad news is many of the patients suffered severe side effects. These include nerve problems with hands and feet going numb. There were also eye problems and abnormalities with red and white blood cells. Use of the drug was stopped before any of the patients suffered permanent damage.
As a result, Chen said more studies are needed to determine whether it can safely be used on a large-scale in combination with other drugs. He also says new, potent antibiotics will be coming on the market and these may be tested on TB, as well.
Extensively drug resistant tuberculosis – or XDR-TB – is still considered rare, although cases have been reported in nearly 80 countries. Health officials believe the number of XDR-TB cases is underreported because there’s no specific test for it.
It can be cured, but the odds against that happening are often quite high. It can kill quickly, especially if a person is co-infected with HIV, the virus that causes AIDS.
Dr. Ray Chen, a staff clinician at the National Institute of Allergy and Infectious Diseases, says XDR-TB is the next step after MDR-TB, or multi-drug resistant tuberculosis, which is a lot more common.
“That’s been a known problem for many years, primarily as a result of people who don’t take their drugs well. And then the tuberculosis bug slowly develops resistance to the drugs that are used,” he said.
MDR-TB is resistant to two of the top line drugs used for standard tuberculosis therapy. When the disease becomes resistant to two additional first-line drugs, it’s upgraded to XDR-TB.
“It came to world attention in 2006 in a study in South Africa where a number of patients were found to have this extensive resistance to tuberculosis drugs, and they had a very high mortality rate. And so it became recognized as a major problem for tuberculosis,” he said.
In fact, the mortality rate was as high at 90 percent in patients also infected with HIV.
Standard TB treatment can take up to six months. MDR-TB treatment can last between 18 and 24 months.
So researchers knew that more drugs were needed to tackle the various forms of TB. They had heard of some informal studies using the drug linezolid on TB patients with some success. But there was no formal study.
Linezolid is a drug that’s already on the market and it’s approved for the use of resistant bacteria, which we call gram-positive bacteria that don’t respond to typical antibiotics.
To find out, researchers tested linezolid on 41 patients with XDR-TB. The patients already had been treated for six months with the best TB drugs available, but failed to respond. Chen said linezolid was added to their regimen.
“We found that adding the linezolid had a significant effect and that most of the patients converted their sputum from showing tuberculosis to not having tuberculosis in the sputum by six months. About 87 percent of the patients became negative for tuberculosis within six months. So it showed a very good response,” he said.
That’s the good news. The bad news is many of the patients suffered severe side effects. These include nerve problems with hands and feet going numb. There were also eye problems and abnormalities with red and white blood cells. Use of the drug was stopped before any of the patients suffered permanent damage.
As a result, Chen said more studies are needed to determine whether it can safely be used on a large-scale in combination with other drugs. He also says new, potent antibiotics will be coming on the market and these may be tested on TB, as well.