For all of the money Americans spend on health care, electronic medical records are still far from universal in the United States.
However, a pilot project in Southern Africa suggests that replacing paper with touch screens may be a good investment in resource-poor countries.
Electronic medical records are not new in Malawi. They’ve been used to track HIV patients for about a decade. Now, a published report describes an expanded version of the program at Queen Elizabeth Central Hospital in Blantyre.
The electronic records system called SPINE, or Surveillance Program of Inpatients and Epidemiology, was set up with three goals. One was to collect what public health officials call “baseline data,” to get a better idea of the medical problems patients are facing.
Miguel SanJoaquin, formerly with the University of Malawi College of Medicine, says a second goal was to monitor changes in health patterns.
“For example, there are issues like how are antiretrovirals working," he said. "Are certain diseases like pneumonia going down because of the introduction of new vaccines, and so on and so forth,” he said in a telephone interview from Cambodia, where he now works.
SanJoaquin says the third benefit is directly aimed at individual patients.
In the past, he said, patients would get a handwritten discharge summary with their diagnosis and follow-up information, such as how to take their medicine.
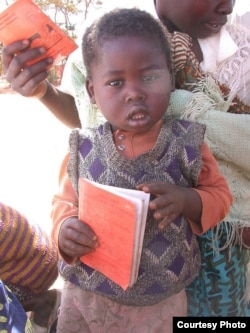
But too often, the writing was hard to read or the information was incomplete. The new system helps patients by giving them a clearly printed discharge summary that is included in a document called a “health passport.”
“Now there is a very neat and clear prescription on a piece of paper that is attached inside their health passport for their benefit.”
SanJoaquin said the information collected gives health authorities new tools to help improve their response to epidemics and other emergencies.
On the other hand, writing in PLOS Medicine, he says that entering the data could be time consuming, and the system was hampered by power outages and hardware and software failures. And that’s in addition to the start-up cost of about $200,000, which was paid by European donors.
Miguel SanJoaquin and his colleagues didn’t do a formal cost-benefit analysis, but they say the experience in Malawi demonstrates the feasibility and usefulness of an electronic medical records system in a hospital with limited resources.
However, a pilot project in Southern Africa suggests that replacing paper with touch screens may be a good investment in resource-poor countries.
Electronic medical records are not new in Malawi. They’ve been used to track HIV patients for about a decade. Now, a published report describes an expanded version of the program at Queen Elizabeth Central Hospital in Blantyre.
The electronic records system called SPINE, or Surveillance Program of Inpatients and Epidemiology, was set up with three goals. One was to collect what public health officials call “baseline data,” to get a better idea of the medical problems patients are facing.
Miguel SanJoaquin, formerly with the University of Malawi College of Medicine, says a second goal was to monitor changes in health patterns.
“For example, there are issues like how are antiretrovirals working," he said. "Are certain diseases like pneumonia going down because of the introduction of new vaccines, and so on and so forth,” he said in a telephone interview from Cambodia, where he now works.
SanJoaquin says the third benefit is directly aimed at individual patients.
In the past, he said, patients would get a handwritten discharge summary with their diagnosis and follow-up information, such as how to take their medicine.
But too often, the writing was hard to read or the information was incomplete. The new system helps patients by giving them a clearly printed discharge summary that is included in a document called a “health passport.”
“Now there is a very neat and clear prescription on a piece of paper that is attached inside their health passport for their benefit.”
SanJoaquin said the information collected gives health authorities new tools to help improve their response to epidemics and other emergencies.
On the other hand, writing in PLOS Medicine, he says that entering the data could be time consuming, and the system was hampered by power outages and hardware and software failures. And that’s in addition to the start-up cost of about $200,000, which was paid by European donors.
Miguel SanJoaquin and his colleagues didn’t do a formal cost-benefit analysis, but they say the experience in Malawi demonstrates the feasibility and usefulness of an electronic medical records system in a hospital with limited resources.