This is Part One of a five-part series on Child Health in South Africa
Continue to Parts: 1 / 2 / 3 / 4 / 5
Amid the noise of crying and moaning children, a little boy lies in a cot, curled up and silent, his eyes staring blankly at the ceiling.
His doctor, Mariaan Willemse, said he’s got a very severe form of tuberculosis meningitis – an extremely dangerous strain of brain TB that’s killing many youngsters in South Africa.
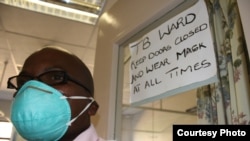
Willemse heads the children’s section of Cape Town’s Brooklyn Chest Hospital. International health experts regard it as one of the world’s leading TB treatment centers.
The hospital is in the epicenter of South Africa’s TB epidemic.
According to the World Health Organization (WHO), the country has the highest rate of new TB cases annually. Thousands of people in South Africa continue to be infected by a disease that’s been virtually eradicated in the developed world.
TB is primarily an illness of poverty. It thrives when people live together in large numbers in close proximity, often surrounded by smoke in small spaces with poor ventilation.
The WHO says every year at least 500,000 babies and children become infected with TB worldwide and an estimated 70,000 die of it – many in South Africa, India and China.
In a recent statement, Dr. Maria Raviglione, director of the WHO’s Stop TB Department, said, “We have made progress on TB: death rates are down 40 percent overall compared to 1990 and millions of lives have been saved.
But unfortunately, to a large extent, children have been left behind, and childhood TB remains a hidden epidemic in most countries.”
Willemse’s hospital is so overburdened with young patients that it cannot help all the children who are contracting TB. “We always have a waiting list. So as the one goes out there’s already somebody (else) waiting to come in,” she told VOA, and added that Brooklyn Chest is thus forced to admit only the sickest children.
Half will die
In adults, TB mostly attacks the lungs. But Willemse explained that in small children, with their undeveloped bodies, it concentrates in the lymph nodes. “This allows the TB to pass more easily into the brain,” she said.
Looking down at another of her tiny patients, Willemse commented, “He was basically in a coma when he arrived here five months ago. Before he got sick, he was a normal four-year-old boy running around. Now he’s cortically blind…His eyes are working but his brain cannot interpret the images…. He’s (deaf) and he’s also a quadriplegic. And at this stage also he’s unable to swallow so he’s being fed with a tube.”
Like many of her young patients, when the boy arrived at her surgery he was unconscious. The prognosis for children with TB meningitis at such an advanced stage is not good, said the doctor.
“Fifty percent of them will die of the disease and the other 50 percent will have severe (brain) damage. They become spastic quadriplegic, meaning that their arms and legs don’t work and are very stiff. They’ll probably have to be looked after at home for the rest of their lives,” said Willemse.
Misdiagnoses
Doctors often misdiagnose TB meningitis, which adds to the pressure the disease is putting on South Africa’s public health system. “It’s easy to mistake it for other common childhood illnesses. It usually starts with just a bit of a headache; the smaller child may be vomiting, having a fever,” said Willemse.
She added that doctors often mistakenly diagnose children who have TB, thinking they have conditions like middle ear infection. They then prescribe antibiotics that obviously don’t heal the youngsters.
“In two days the child is still not eating, is still vomiting, is now starting to become very sleepy, lethargic, and doesn’t want to play anymore. But the mom often (doesn’t) go back to the same (doctor) because it didn’t work (the first time) so she goes somewhere else – up until the child has convulsions. And then they know that this is something serious….”
But by this stage, said Willemse, it’s often too late to save the child from permanent disability, or even death.
She said that perhaps the most difficult part of her job is to tell parents that their previously healthy child will never be the same again, because of TB meningitis.
“I can’t tell them upfront, ‘Your child won’t be able to walk or won’t be able to sit.’ I can’t say that, but I can tell them that ‘I already see there is a lot of brain damage. And I already know that your child is not going to be normal; your child did have severe damage.’ And that’s not nice at all. It’s a heavy burden sometimes. One sometimes lies awake at night, and you pray for them.”
‘A manmade disease’
In another corner of the hospital’s children’s ward, Willemse gestured towards an infant in a cot and explained, “She’s six months old. She’s been here for a month. The mommy died two days after the baby was born. She was born very prematurely. This child’s mother had TB while she was pregnant.”
The mother infected her child with another potentially fatal kind of TB, namely multidrug resistant, or MDR, TB. “It’s a manmade disease,” said Willemse. It has developed as a result of people with normal TB not completing their treatment.
“The drugs have side effects, such as nausea, and so many people stop taking them. Many adults default with their treatment, after which the TB germ develops resistance to the routine antibiotics with which we treat the condition,” the doctor explained. “They then infect their children with MDR (TB).”
Six months of treatment usually wipes out normal TB. But MDR TB patients need 18 months of medication to heal. They’re hospitalized and injected with drugs for six months, followed by 12 months of treatment at a local clinic.
The injected medicines have dangerous side effects, especially for very young patients. They can make the children go deaf. They can damage their kidneys and their thyroid glands.
But Willemse emphasized that the drugs still offer MDR TB sufferers’ the best chance of survival.
Losing the battle
After decades of government programs, as well as local and international interventions aimed at ending South Africa’s TB scourge, Willemse sees no sign of it abating soon. In fact, based on her experience, she said it’s getting worse.
“More than half of the children admitted to Brooklyn Chest have MDR TB, and that’s just the tip of the iceberg. We are losing the MDR battle,” she said.
Giving reasons for this, Willemse said cases of MDR TB aren’t picked up in time at South African clinics. In addition, TB patients aren’t being counseled properly at many public health facilities. As a result, she said, they don’t realize how infectious the disease is and how important it is for them to complete their treatment - and how easily they can pass TB on to their children.
Willemse said TB patients themselves are also responsible for spreading the disease. “I think the crux is that the adult who is coughing and losing weight must go to the clinic and must be tested for TB. But it’s a major problem that there are people who are still unwilling to be tested.”
Willemse said TB infection rates in South Africa will drop in the future if health services improve but predicted that the country will never be a TB-free society.
There’s too much poverty, she said, and this means the conditions that allow TB to thrive will endure well into the future.
More than 1,000 miles away from Brooklyn Chest Hospital, another doctor, Taryn Gaunt, is also dealing with a flood of TB cases in Oliver Tambo District.
She said, “South Africa can implement all the interventions it wants to fight TB. But at the end of the day, only when the standard of living radically improves in the country will we be able to talk about the possible eradication of TB. Until them, we’re locked into this terrible cycle where we invest so much money in trying to fight a disease that just seems to have no end.”