Two teams of scientists, working independently, have developed a way to give a patient multiple cancer drugs simultaneously, to see which works best.
The two groups have different approaches, but each starts with the premise that it’s best to test anti-cancer drugs in the living tumor.
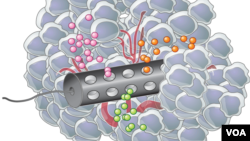
At the Massachusetts Institute of Technology, the result is a very small device that can be placed inside a tumor. Though it’s less than a millimeter in diameter, it has 30 to 40 tiny reservoirs containing different drugs that interact with adjacent tumor cells.
Then, after a day or so, team leader Prof. Robert S. Langer said a biopsy needle is used to retrieve the device.
“You not only take out the device, but you take out the surrounding tissue around the device. And then you can look at what’s happened to that tissue," said Langer. "You can see how the different drugs have performed. And that tells you what we believe will be the best cancer chemotherapy regimen in that patient.”
Treating cancer is not a one-size-fits-all proposition. Some cancers that respond to a particular drug in some patients don’t help at all in others.
Langer said testing drugs on a tumor which is in the patient’s body can give better results than trying out the drugs in the laboratory on tumor cells that have been extracted from the patient.
“The fact that you take something out, it’s no longer in its natural habitat - and certainly lots of people have shown that cells, once you take them out of a patient, don’t behave necessarily the same way they do when they’re in the patient,” he said.
Trying out different drugs, or drug combinations, on a small scale right in the patient’s tumor can help doctors tailor the treatment to the person.
“It couldn’t be more personalized,” is how Langer puts it.
Another group tackling the problem is Presage Biosciences, a Seattle company. Their approach is different, but in a promotional video, company president Nathan Caffo agreed about the importance of personalization.
“That’s the sort of thing that’s going to help us understand how patients are similar, how they can be treated similarly, and how we really shouldn’t treat patients all the same,” he said.
The Presage device, called CIVO, has been tested in several human patients.
The MIT device is heading for human trials, probably in about a year. Both devices are described in the journal Science Translational Medicine.